The annual Health and Care Innovation Expo took place in Manchester from 11-12 September. Lyn Whitfield from Highland Marketing reports on the key speeches and announcements, as the NHS gears up for a tough winter
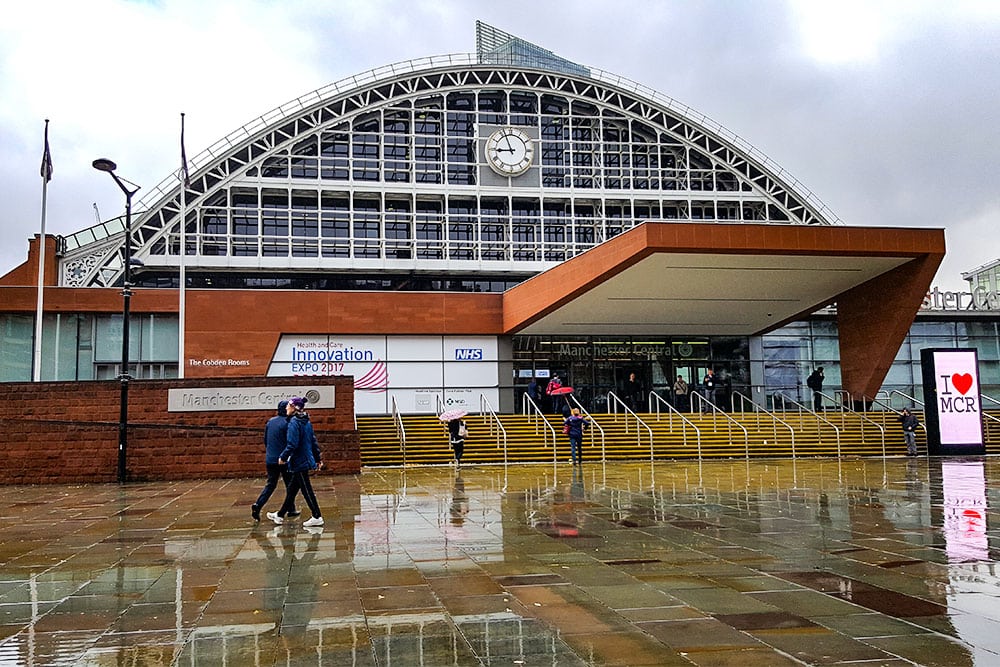
Visitors to the Health and Care Expo in Manchester could be in no doubt that winter is coming. As they made their way to Manchester Central, visitors were lashed by Storm Aileen.
Once they were inside the convention centre, they were repeatedly urged to make sure their services were on top of their winter planning. Just to add to the sense of urgency, NHS England chief executive Simon Stevens warned that a major flu outbreak could be on the way.
“The signs from Australia and New Zealand, which are just coming out of their winter, are that it has been a heavy flu season, and many hospitals have struggled to cope,” he said. “So let’s work together, over the next six to eight weeks, to put the NHS on the right footing for the winter ahead.”
Winter’s coming
This will be a challenge. Over the summer, Jim Mackey, the outgoing chief executive of NHS Improvement, said he was “surprised” by how “very fragile” some trusts had been last winter, and by how much support they had needed.
Also, by how much extra beds and staffing had knocked acute finances. At Expo, NHS England national director of operations and information Matthew Swindells reiterated Mackey’s message that this could not happen again.
The health service is heading into the first of the two ‘lean years’ of its five-year settlement so, he said, trusts need to keep on top of their control totals and to keep checking the assumptions behind and the progress of their savings plans.
“There is no point rolling the dice again and hoping there will be more money,” he said. “We know what the financial totals are.”
Finding the money
In the longer-term, the NHS’ hope of escaping from this unremitting demand and financial pressure are bound up in the 44 sustainability and transformation plans that have been drawn up to implement the Five Year Forward View plan that was launched in 2014 to close a £30 billion funding gap by 2020-21.
Swindells acknowledged the plans are variable; with some much more developed than others. But he said the basic idea was to remove incentives for some organisations to generate activity at the expense of others, and to create “permission” for systems to tackle problems together.
He also argued there are big savings to be had. The NHS RightCare programme, which advises systems on how to use data and new care concepts to improve efficiency by getting patients to “the right care, in the right place, at the right time,” has estimated that it could generate £2.4 billion.
The Getting It Right First Time programme, which is focused on reducing variation in clinical quality, has estimated that it could generate £3.4 billion.
“These are not cuts. This is money that is available to put into things that the public we serve have a right to expect,” Swindells said. “What we need is brave leadership to make it happen.”
Defending and expanding the GDE programme
Leadership and, of course, innovation. On the IT front, the big game in town is the global digital exemplar programme, which was launched almost a year ago, following the Wachter Review of NHS IT.
The programme created 17 acute GDEs, each of which will receive £10 million to make their own IT “world class” and to support others.
At a ‘digital transformation leadership panel’, NHS chief information officer Will Smart acknowledged that the programme was not “widely welcomed, because people felt it focused on a handful of favoured institutions.”
However, he argued that it’s influence has spread, with seven mental health GDEs added and an ambulance programme on the way. In addition, health secretary Jeremy Hunt was able to announce 18 acute ‘fast followers’ at the end of the show [see highlights].
Back in the ‘digital transformation’ session, outgoing NHS chief clinical information officer Keith McNeil made a considerably more robust defence of the GDE programme.
“I think we have the chance to be proud of what we are doing, and we will not do that by miring ourselves in mediocrity,” he said. “The GDEs are setting the bar, and saying ‘this is what we want’ on behalf of the whole health service, and therefore patients.”
McNeil also had little sympathy for a questioner who asked what support was available for less digitally mature organisations. “I think the reason [some] trusts are less digitally advanced than others is that they have not put in the investment,” he said.
“So we need to provide some resource to get transformational leadership in there, and then trusts have to stand up and put up. One of the things they just have to do is put money into transforming digital at their organisations.”
Swindells issues IT challenges
McNeil’s reference to “investment in transformational leadership” related to the NHS Digital Academy, another outcome of the Wachter Review that was also launched at this year’s Expo, initially to train a new generation of CIOs and CCIOs, who like to see themselves as the “rock stars” of healthcare IT [see highlights].
His wider point, that trusts need to spend on technology, and start seeing it as an investment rather than a cost, was echoed by Swindells; who said his challenge to NHS managers was to “work out how to build IT into your business strategy.”
He put up slides of patient pathways, showing where IT might be used to divert patients, cut costs by allowing them to do their own booking, improve efficiency by allowing services to share records, or improve quality via decision support.
Being Matthew Swindells, he also issued two further challenges: one to IT departments to “get out and explain how IT can be used to change care”; and one to vendors to “be open.”
“Vendors should not be locking down data, and hospitals should not be treating their data as a market opportunity,” he said. “That is not what the NHS is.”
He said he would not be afraid to get tough on vendors or to “make it clear who is sharing and who is not”. He also urged the NHS not to buy from vendors who refused to interoperate and “not to take any sh*t” on the subject (for which he looked mildly embarrassed).
Tech: a new hope
How does any of this help the NHS to prepare for that tough winter that is coming, though? Swindells was asked this towards the end of his keynote session.
He suggested the answer was to look at where innovation could divert people from A&E and GP surgeries; but also to make sure that people knew about schemes and used them. Quietly, this was something of a theme at this year’s Expo.
In an oddly titled session on ‘the NHS as a digital exemplar’, for instance, participants discussed some of the other IT initiatives that are already under way in the NHS, from the revamped NHS App Library, which now has 43 apps, to the controversial ‘data lakes’ that will release anonymised data for analysis.
When a commissioner in the audience asked how she could set about “landing” some of this technology in “business as usual activity”, the panel’s advice was to start with what is already available, and get that working as well as possible.
Bruce Greenstein, the chief technology officer at the US Department of Health and Human Services, said the answer was not to look for “Star Wars Technology” but to “start using what is out there.”
Juliet Bauer, the chief digital officer at NHS England agreed, with the caveat that it was important not to replicate existing services as digital services; but to create new forms of access that will “allow people like my mother to go online and just sort whatever problem they have.”
Eight digital challenges for NHS England
More innovation is on the way, though. With his winter warning delivered, Stevens outlined a raft of investments to help the NHS adopt new drugs, make better use of anonymised clinical data, drive the adoption of AI, and deploy new but proven medtech by expanding the innovation tariff [see highlights].
And, shortly afterwards, Jeremy Hunt in his almost totally tech-focused speech, not only announced the 18 GDE fast followers, but ticked off eight digital challenges for NHS England.
These were: getting NHS 111 online and on apps; aligning the NHS symptom checkers with NHS 111; launching a new NHS app [see highlights]; driving use of appointment booking online; driving use of repeat prescriptions online; getting the consent app promised by the latest Caldicott Review of NHS security and information governance up and running; enabling people to record their organ donor preferences online; enabling people to record their end of life preferences online; expanding the revamped NHS App Library; and expanding the NHS’ digital inclusion programme [see highlights].
Quite a big programme; albeit one the NHS is already tackling, and has been doing for some years. However, Hunt also concluded by looping back to the idea that all this technology has to have a purpose: helping to create “the safest, highest quality health system in the world.”
“As we grapple with the challenges [that face us], technology can be our friend, if we recognise it is a means to an end, and not an end in itself.”