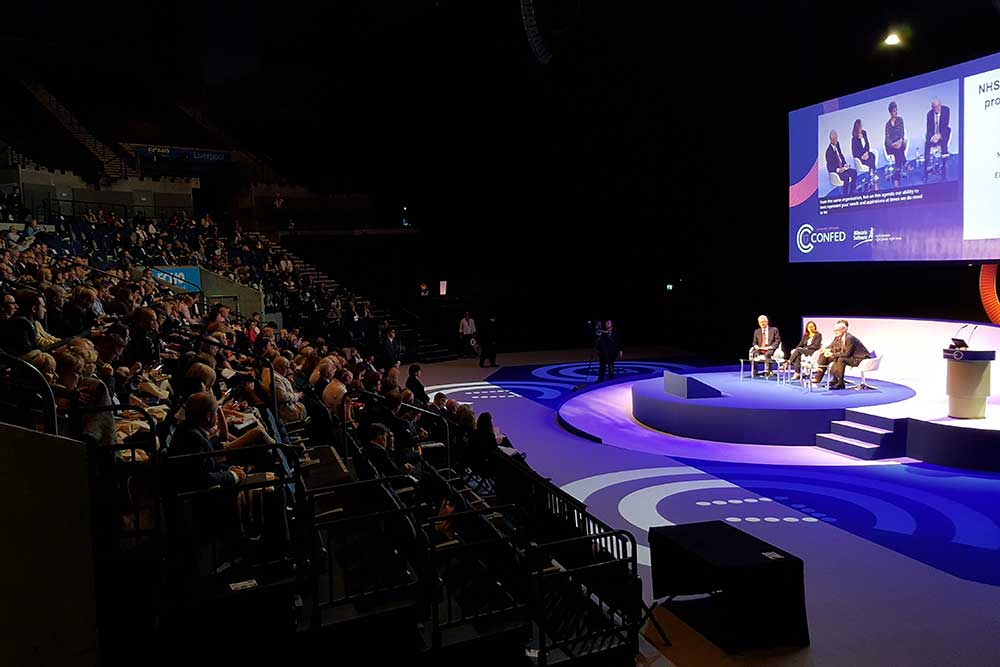
The NHS Confederation held its annual conference in Liverpool last week. Lyn Whitfield gives a flavour of the event, and where it leaves the NHS as it finalises funding plans, gets ready for Brexit, and starts the third year of the Five Year Forward View.
The NHS Confederation’s annual conference in Liverpool was sandwiched between the general election and the start of Brexit negotiations. So, naturally, the question running through its sessions was what they would mean for the NHS, its finances and reform agenda.
The general election: Victoria MacDonald, the health correspondent for Channel 4 News, told an opening debate there were some positives from the election, which left Theresa May leading a minority government with an almost unchanged cabinet.
“Without wanting to sound too much like Theresa May, I do think the NHS needs some stability,” she said. On the other hand, the campaign had failed to ignite around health and care, when both “could do with some fresh thinking.”
Paul Stephenson, an aide to former health secretary Andrew Lansley, who played a prominent role in the Vote Leave campaign, felt it was worse than that. The NHS is supposed to be pushing forward with the Five Year Forward View to save £30 billion by 2020-21 through a combination of efficiency and new models of working.
Yet the legislation that might be required to implement the more radical ideas is all but off the agenda, thanks to the weak government and the demands of Brexit, he said.
Also, MPs may look at Canterbury, where Labour’s Rosie Duffield won by 187 votes on a ‘save’ Kent and Canterbury Hospital ticket, and back away from the sustainability and transformation plans that are meant to translate the FYFV into local action.
Also, “serious social care reform is off the agenda” after the disastrous ‘dementia tax’ proposal in the Tory manifesto. “If you think stability and politicians staying out of the NHS are good things, then it was a good result,” he said. “If you think the NHS needs serious reform, then it was a very bad one.”
Brexit: Stephenson was quizzed about the infamous ‘Brexit bus’ poster that promised £350 million a week for the NHS – £19.7 billion a year, or just less than the £22 billion that it needs to generate through the FYFV (with the other £8 billion coming from the Treasury).
He said he thought the government should deliver the cash, because “it would fix a lot of the demand pressure on the NHS”; but this was unlikely to happen because the health service “tends to be seen as guilty of special pleading.”
So, if Brexit is unlikely to deliver significant, additional cash to the NHS, what other impacts could it have? Another panel argued there were real concerns about workforce, given that the Health Foundation has shown that the number of EU nurses registering in Britain has already dropped dramatically.
Also for procurement, since it’s no longer clear what rules will operate, for medicines, since other countries will bid to host the London-based European Medicines Agency as early as July, and for research, since the UK will find it harder to access EU research projects.
The NHS Confederation has helped to create a new alliance, the Brexit Health Alliance, to try and safeguard the health service’s interests as talks get underway, with workforce top of its list.
Workforce: Not that Brexit is the only pressure on the NHS workforce. Ian Cumming, the chief executive of Public Health England, noted that while the number of clinicians in the NHS has risen since his organisation was created in 2012, there are still tens of thousands of doctor and nurse vacancies.
Worse, many older staff are desperate to retire, while younger ones may leave within a few years of starting their careers or opt to work fewer hours than the generations before them.
Cumming urged his audience to address “retention, retention, retention”. Other leaders at the conference urged the government to drop the seven-year pay cap that has depressed wages and morale.

The financial crisis: The obvious problem to lifting the pay cap, however, is that holding down wages has been one of the NHS’ more effective responses to its immediate financial crisis.
Jim Mackey, the outgoing head of NHS Improvement, had some relatively good news on this front. In his keynote address, he congratulated the NHS for managing to finish 2016-17 in balance, thanks to “a fantastic effort by providers, doing incredible things” to get their deficit down to £791 million (after a £1.8 billion bailout).
He indicated that the provider sector will be heading for a deficit of £500 million this year, once trusts have signed up to their ‘control targets’. So now the NHS ca n focus on “a big push on productivity”, winter planning, and the FYFV agenda.
If Mackey had a message, it was that things are grim, but the NHS is getting there. “People will write books about this period,” he concluded. “And they will not be about ‘the end of the NHS’ but about how you all did the impossible, and made it sustainable for the future.”
STPs and ACOs: An alternative view, that things are just grim, was on offer at a session organised by NHS Providers, whose leader, Chris Hopson, has spent the last two years arguing that STPs won’t work, at least without significantly more money.
Siva Anandaciva, chief analyst at the King’s Fund, told the session the NHS had three “bullets” to try and close its funding gap by the end of this Parliament. These were pay restraint, new models of care and efficiency. Like so many others in Liverpool, Anandaciva felt pay restraint was no longer realistic.
He had good and bad news on new models of care, drawing on research from the US, which has already introduced accountable care organisations to deliver population-level funded, integrated care. The good news is that ACOs deliver better quality; the bad news is that “they do not take cost out of the system quickly.”
Efficiency: So, that leaves efficiency. Jim Easton, the Department of Health’s former director of improvement and efficiency, who now heads Care UK, a private provider of NHS 111 and orthopaedic services, told his former colleagues that they needed to focus on procurement, time saving, and technology.
He told them they continued to spend “far too much” on common supplies and that they were “unnaturally relaxed” about “small wastes of time, like a five-minute theatre handover” when “cutting that out is half your annual savings target.”
Easton also urged his audience to start using technology like other industries, to shift administration costs onto users. “Banks and airlines do it, and we love it, because it puts us in control,” he said. “Patients would love to do some of your administration for you, and you won’t let them.”
IT: Unfortunately, this was one of the few mentions of IT at the conference. Companies used break-out sessions and the exhibition floor to highlight the work that some trusts and cities are doing on electronic patient records and information sharing.
NHS Digital also sponsored a stream, but its interim chief executive Rob Shaw found visitors were more interested in the WannaCry #nhscyberattack than anything else. He argued that the NHS had coped “really, really well” with the ransomware incident, but needed to do more on “first hour communications” and lining up support for trusts that needed to “call in the cavalry” in future.
Keynotes: Niall Dickson: So, where does the NHS stand at what Niall Dickson, the NHS Confederation’s new chief executive, called “the dawn of a new, if somewhat fragile Parliament”?
Dickson pointed out that the past five years have seen “the biggest increase in population since 1945” and a “step change in demand” because of aging. Funding increases have been historically low, yet the NHS has been “remarkably resilient” and “the books are balanced.”
The question is whether it can keep going, given the ongoing age shift of the population and new challenges, including Brexit. Dickson cast doubt on this. He argued the STP process had been “difficult” and “the reality of sustainability can overwhelm transformation on the ground.”
He argued it is time for a political “reset” for the NHS, for the Conservatives to deliver on their manifesto pledge of more money and, in the longer term, for a defined percentage of GDP to go on health and care. Also, for politicians to “engage consistently on changing services” and to lift that pay cap.

Hunt and Stevens: There are few signs this will happen. In his keynote address, health secretary Jeremy Hunt paid tribute to the NHS staff who worked during the Manchester and London terrorist attacks, and the fire at Grenfell Tower.
But after that, he outlined just two priorities for the health service; delivering the four-hour A&E waiting time target and keeping on top of the finances. “As Jim Mackey said, provider performance has been terrific, but [the acute sector] deficit should never have reached £2 billion [as it did in 2015-16],” he said.
The deficit had set back the FYFV by a year and financial control was now vital to “invest in the transformation plans that we all know are essential to the future of the NHS.” Hunt did say he was willing to talk to the Chancellor about the pay cap, capital funding and more money for the NHS “as the economy allows.”

NHS England’s chief executive, Simon Stevens, barely promised that much. There was a plan for the NHS’ problems, he said shortly before delegates left Liverpool, and “that plan was published in March, and it is the Next Steps on the Five Year Forward View, and it is unaffected by recent developments.”
STPs are “very much the direction of travel” and eight accountable care systems are about to come on stream. But the plan depends on keeping control of the money. “So as Jim Mackey said, congratulations on balancing the budget, but the bad news is that we need to do it all again.”
Keep on keeping on, in other words. Or, as Stevens advised his audience: “Stay focused, stay practical, and stay positive.”